Optimizing Emergency Department Scheduling in Real-Time
The Need
 Emergency Departments are faced with many challenges, not the least of which are overcrowding and understaffing. For ED medical directors, the problem of emergency department scheduling is not only having enough staff scheduled, but having the right staff at the right time to treat the right patients. Patient arrivals can be highly variable, with sudden fluctuations in volume from hour to hour, different types of patients arriving during different times of day, vastly different patterns by day of week, and even seasonal changes associated with flu, school calendars, and local demographics. Traditionally, coverage schedules are planned based on volumes of patients, averaged over large periods of times, with little consideration to this variability – and often simply by gut hunch. This can lead to over coverage during some hours of the day, representing substantial financial loss, and can lead to under coverage at other times, leading to long times, high walk-out rates, and risks to patients.
Emergency Departments are faced with many challenges, not the least of which are overcrowding and understaffing. For ED medical directors, the problem of emergency department scheduling is not only having enough staff scheduled, but having the right staff at the right time to treat the right patients. Patient arrivals can be highly variable, with sudden fluctuations in volume from hour to hour, different types of patients arriving during different times of day, vastly different patterns by day of week, and even seasonal changes associated with flu, school calendars, and local demographics. Traditionally, coverage schedules are planned based on volumes of patients, averaged over large periods of times, with little consideration to this variability – and often simply by gut hunch. This can lead to over coverage during some hours of the day, representing substantial financial loss, and can lead to under coverage at other times, leading to long times, high walk-out rates, and risks to patients.
In our role as a Physician Support Resource, we set out to address this problem, specifically as it pertains to Physician and APP staffing for our client physician practices. We sought to answer the question for our clients –
“How do we optimize provider schedules in an objective and systematic approach that reflects the realities of the Emergency Department?”
The Data
As a data-driven company, Intermedix has long collected detailed information on our client practices. Billing data, staff schedule data, hospital registration data, and patient tracking data are core components of our Practice Management Platform. We also have a long tradition of applying statistical analysis, simulations, and predictive models to practice management problems. Traditional approaches to coverage planning rely too heavily on average or aggregated data, which prevents a medical director from taking into account the inherent variability they are faced with. Therefore, granular data was chosen as a foundation for this new approach.
Working with patient level data also allowed us to address the issue regarding patient acuities. It’s long been recognized that acuity levels vary in semi-predictable ways by hour of day, day of week, and week of year. Older, sicker patients tend to arrive during morning hours, with lower acuity, younger patients arriving in the evenings. Mondays see more arrivals from nursing homes. Fridays see more traumas. By incorporating RVU data from each patient record, acuity would automatically become part of the calculations.
Knowing that hours actually worked by providers frequently deviates from scheduled coverage, the Intermedix data platform integrates actual hours worked for each provider. This in turn gives us a robust picture of provider productivity for every hour of the year, matched to patient types, and even by hour of a given shift for a particular provider.
The data though only serves as a history. It allows us to look back to see what happened, albeit with a precise level of detail. In order to optimize schedule definitions, a medical director must be able to do “what if” scenarios. “What if I start B Shift an hour earlier?” “What happens if volume increases 5%?” “Would a mid-day MLP shift on Mondays help?” “How much could we save by cutting a double coverage shift?”
To create this capability, we turned to another of our core expertise – software.
The Tool
Using the data as a foundation, software specifically tailored for the use by our client medical directors was designed. We borrowed a page from industrial engineering and incorporated analytic views using a demand load versus resource capacity model. Thus the “Tool for Optimizing Provider Schedules” – TOPS – was born. TOPS presents the medical director with a series of control panels that manage the load of historical data and current schedule definitions, configuration of parameters such as hourly rates and anticipated volume changes, the display of calculated values such as provider productivity, and of course the ability to add, change and remove shifts.
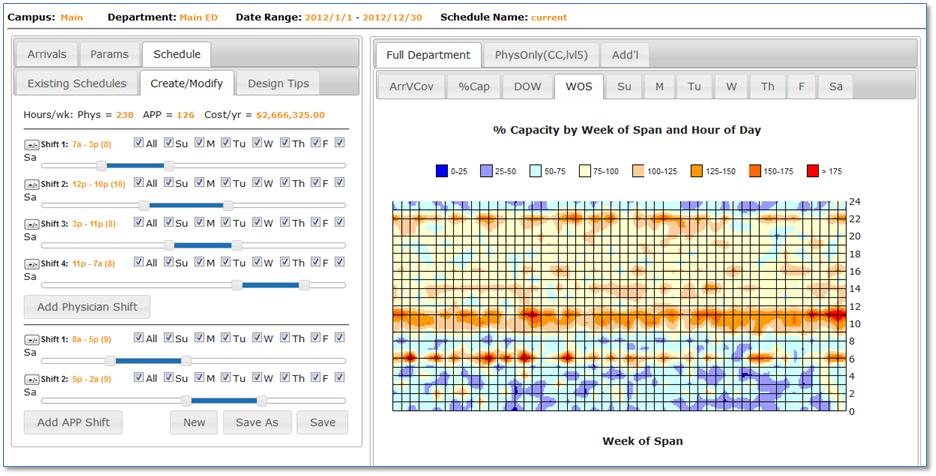
Data, parameter, and schedule changes are immediately reflected in the various graphical views displayed side by side with the controls. These views give the medical director immediate insight into proposed changes, including impact by hour of day, day of week, and week of year. Variability is also addressed by giving frequency histograms of percent over capacity events. Arrivals are also broken down by the type of provider that can see the patient, creating separate capacity views for “Physician Only” patients as well as the department as a whole. Shift capacity can be modeled using either blocked (flat) productivity assumptions or sculpted capacity that takes intra-shift provider productivity into account. Proposed schedules can be saved off and referenced later as well as shared with other users within the same practice. Costs associated with each schedule are displayed right on screen for quick comparison.
The Results
TOPS has now been in use by dozens of EDs across the country and our clients have realized real cost savings. As importantly, client physicians consistently tell us the power of being able to fine tune their schedules both in terms of patient quality of care – right staff at the right time for the right patient – and in terms of physician work load. With TOPS always available, practices can rapidly adjust their schedules as conditions change, eliminating the guess work previously required. In addition, TOPS gives the medical director an objective, quantifiable information to share with the hospital in aligning nurse and tech staffing with patient load.
The Future
We will continue to enhance and refine TOPS as the ED environment changes as well. First in priority is the integration of real-time predictive models that forecast ED arrival volume WITHIN a day based on immediately prior arrivals. We have also developed seasonal predictive models for rapid spike volume drivers such as flu. Integrating these models with TOPS will be one-click away with future releases. In addition to the ED, we are also in the process of adapting TOPS to address the needs of additional hospital based physician specialties.
We see this kind of data driven, software integrated approach to practice management as an essential strategy for physicians in the quickly changing world of healthcare.
We invite you to view a complete listing of our current clients. If you are a physician or advanced practice provider interested in working with an independent, democratic emergency medicine group we'd love to speak with you about your career needs.